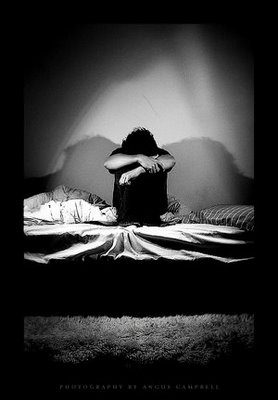
Soldiers Report PTSD Symptoms and Other Mental Health Problems

ABCNews Medical Unit
 Even though he’s retired from active military duty, CSM Samuel Rhodes still suffers from deep emotional wounds.
Even though he’s retired from active military duty, CSM Samuel Rhodes still suffers from deep emotional wounds.
“I had to take this afternoon off from work today because of anxiety,” he said. “And sometimes, if I’m going through a really tough time, I think about suicide.”
He spent nearly 30 years in the Army and recently spent 30 straight months deployed in Iraq where he, like many soldiers, witnessed some of the horrors of war.
“In April 2005, it started to eat me up because I started losing one soldier after another,” Rhodes said. “We lost 37 soldiers that were in my unit.”
He was in charge of the brigade of 37 soldiers, and as time wore on, the loss of life wore him down.
“In April 2007, it came full circle. I considered suicide as an option. I felt guilty about losing those soldiers, even though I had no control over it,” he said.
“And I was sleepwalking. I had to tie myself to my cot to prevent it,” he added.
Later, during his 24th month in Iraq, he was found unconscious, and doctors diagnosed him with exhaustion. At that time, the combat stress doctor told him he was also suffering from post-traumatic stress disorder.
“He started explaining it to me, and I realized he was right,” Rhodes said.
And according to a new study conducted by researchers at Walter Reed Army Institute of Research, Rhodes’ mental health problems are common among soldiers returning from Iraq.
Between 2004 and 2007, researchers gave out anonymous surveys to four active duty brigade combat teams and two National Guard combat team three months and 12 months after deployment. The surveys screened soldiers for PTSD, depression, alcohol misuse and aggressive behavior and asked them to report whether these problems impacted their ability to get along with others, take care of things at home or perform their job duties.”A high number of those that had symptoms of PTSD and depression also reported some aspect of impairment,” said Jeffrey L. Thomas, one of the study’s co-authors. “The range was about 9 to 14 percent.” Depression rates ranged from 5 percent to 8.5 percent.
But by using a less stringent definition of PTSD, they found between 20 and 30 percent of soldiers showed symptoms of PTSD, while they found between 11.5 to 16 percent of them were depressed.
Full article, please go to: http://abcnews.go.com/Health/MindMoodNews/10-soldiers-fought-iraq-mentally-ill/story?id=10850315&page=2