By Carlene Hill Byron
How many families in your church have a loved one who struggles with mental health problems? That’s kind of a trick question. People don’t talk about mental health problems. You’re more likely to hear them describe their child’s condition as “something like autism,” as the elder of one church we know says.
Or they might cover up entirely, as does an elder’s wife in another congregation. When her bipolar disorder swung into mania after childbirth, her family, already managing the added responsibilities of a newborn, had to manage her condition as well. But because her condition is a secret, they did so without any support beyond the usual “new baby” dinners.
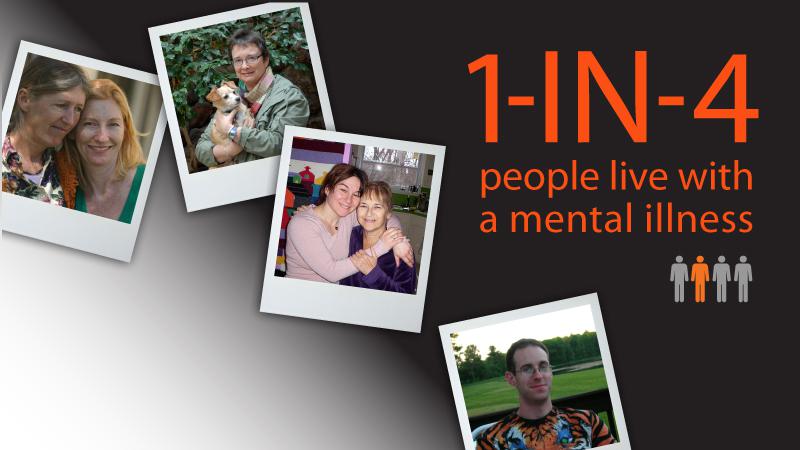
The answer to the question is, if your congregation is representative of the U.S. population, one in four households will struggle with someone’s mental health problems over their lifetime. That’s schizophrenia, bipolar disorder, obsessive compulsive disorder, disabling chronic depression, and various anxiety disorders. Look at the faces seated around you this Sunday. Someone is probably hurting. And they’re probably afraid to tell you.
The least acceptable disability

A study where people ranked disabilities by their “acceptability” returned these results, in order–most acceptable: obvious physical disabilities, blindness, deafness, a jail record, learning disabilities, and alcoholism.
Least acceptable: mental health problems. People with mental health problems frighten us because when people become mental ill, they become someone we don’t know. A bright boy who was his family’s bright hope may find he just can’t cut it anymore as schizophrenia turns him paranoid, disoriented, unmotivated in the extreme, and overwhelmed by delusional voices that tell him, over and over, how worthless he is.
Or, in the case of bipolar disorder, a girl who was a well-liked and active member of her Teen Challenge group may suddenly turn promiscuous, run away from home, and make a new home in the streets of a strange city. Laziness. Promiscuity. Violence. Sin. That’s what many people see when they look at those with mental health problems. It’s hard to believe that people may behave in such unacceptable ways and not be in control of their behavior.
Having a mental health problem is a lot like being on alcohol or drugs, without being able to stop. Medications “work” for about two-thirds of us. That means that a third of us can’t ever get off the chemical ride that our brains produce.
For those of us who can use medications, the side effects can be daunting. I have lost about 20 percent of my small motor functionality as a result of one of the five medications I take for bipolar disorder. I prefer that to losing large motor control and having another auto accident, being so disoriented I can’t find my way home from the store, losing bowel control in a busy bookstore, gaining 45 pounds, or any of dozens of side effects I’ve experienced on other medications.
Many people become so frustrated with side effects that they stop taking medications. Only about half of us accept treatment. Even when we are treated, not everyone regains their status as a fully functioning adult. In our extended family, six people have diagnoses. Those with bipolar disorder and chronic depression are successfully medicated and work full-time. Those with panic disorder and schizophrenia are on permanent disability. Nothing has pulled them through.
What the Bible says
The Bible talks about mental illness, as well as physical illness.
- It describes a king who was made mentally ill until he would recognize the sovereignty of God (Dan. 4:29-34).
- It describes demonized men who lived among the tombs and terrorized everyone until Jesus set them free (Matt. 8:28-33).
- It also describes as demonized a young boy that most scholars today say had epilepsy (Matt. 17:15-18). Jesus delivered him, too.

What does this tell us about illness?
First, that God is able to heal. Second, that some physical and mental illnesses are caused by demons. Third, that some mental illnesses are caused by sin. But are all mental illnesses caused by demons or sin, and is seeking God our sole resource for physical and mental healing?
Since the 1950s, we have usually sent church members with epilepsy to doctors for effective treatment with anti-convulsant drugs. In a similar way, we’ve learned that medicines can effectively treat many cases of mental illness. So if all mental illnesses were caused by demons and sin, medicine would be exorcising demons and turning hearts to repentance. That is certainly untrue, for those are the works of the Holy Spirit.
Instead, we now know that most if not all mental illnesses are biological in origin, with environmental factors possibly triggering an existing genetic predisposition to the illness. Mental illnesses, just like epilepsy, are biological disorders of the brain.
What can the church do?
Compassionate service is one of our core charges as Christians. We observe it almost daily in the experience of one man we know with schizophrenia. His life is confined almost entirely to his home due to the fear, indecision, and lethargy that have become the shape of the illness in his body. But neighbors bring him occasional meals. The secretary of his small church talks to him by telephone every weekday. Several other members take weekly calls at designated times to help break his isolation. If he doesn’t feel up to driving to his Bible study meeting or Sunday services, some member will give him a ride. Nearby relatives help him plan and manage his finances, and come by to clean occasionally and for DVD “movie nights.” Phone cards given as gifts allow him to call his mother nightly. There’s much more that could be done—more frequent house cleaning and more meals and more visits—but he enjoys far more contact with many more loving people than many shut-ins.
The challenging good news is that when people with mental illness turn to someone outside “the system” for help, the church is first to get the call 40 percent of the time. Is your church ready?
…………………..
Carlene Hill Byron is the former Director of Communications for Vision New England. Through NAMI—the Nation’s Voice on Mental Illness, she and her husband, James, train churches to effectively serve people within the congregation with mental health problems and also teach NAMI’s class for families of people with mental health problems. They are members of Asbury United Methodist Church in Raleigh, North Carolina, where James serves on staff. First published by Vision New England’s Ministries with the Disabled, Acton, Massachusetts.
http://www.mentalhealthministries.net/index.html
Related articles
- The Gifts of Bipolar Disorder (acanvasoftheminds.wordpress.com)
- He ain’t heavy, he’s Bipolar (acanvasoftheminds.wordpress.com)
- Police are learning to deal with the mentally ill (kansascity.com)
- Warning: This post contains mental health issues (tryingtowriteit.com)