Definition by Mayo Clinic staff
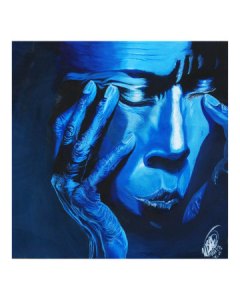
Depersonalization is a sense that things around you aren’t real, or the feeling that you’re observing yourself from outside your body. Feelings of depersonalization can be very disturbing and may feel like you’re losing your grip on reality or living in a dream.
A lot of people have a passing experience of depersonalization at some point. But when feelings of depersonalization keep occurring, or never completely go away, it’s considered depersonalization disorder. Depersonalization disorder can be severe and may interfere with relationships, work and other daily activities. It will sometimes ‘piggyback’ on other mental disorder, like Bipolar or PTSD.
Depersonalization disorder symptoms include:
- Continuous or recurring feelings that you’re an outside observer of your thoughts, your body or parts of your body
- Numbing of your senses or responses to the world around you
- Feeling like a robot or feeling like you’re living in a dream or in a movie
- The sensation that you aren’t in control of your actions, including speaking
- Awareness that your sense of detachment is only a feeling, and not reality
Other symptoms can include:
- The sense that your body, legs or arms appear distorted, enlarged or shrunken
- Feeling like you are observing yourself from above, as if you were floating in the air
- Feeling emotionally disconnected from people you care about
While episodes of depersonalization may last only a short time, some people with depersonalization disorder have episodes that last hours, days, weeks or even months at a time. In some people these episodes turn into ongoing feelings of depersonalization that may periodically get better or worse.
When to see a doctor
Passing feelings of depersonalization are common, and aren’t necessarily a cause for concern. But ongoing or severe feelings of detachment can be a sign of depersonalization disorder or another physical or mental health condition. See a doctor if you have feelings of depersonalization that:
- Are disturbing you or are emotionally disruptive
- Don’t go away, or keep coming back
- Interfere with work, relationships or daily activities
- Disrupt your family
Depersonalation can last just a few hours or more. It is believed that this is a response to anxiety—as the root cause. Panic attacks (acute anxiety) are often the culprit behind DP,
Useful Depersonalization Sites (That I can recommend)
https://my.clevelandclinic.org/health/diseases/9791-depersonalization-derealization-disorder
http://www.mayoclinic.com/health/depersonalization/DS01149