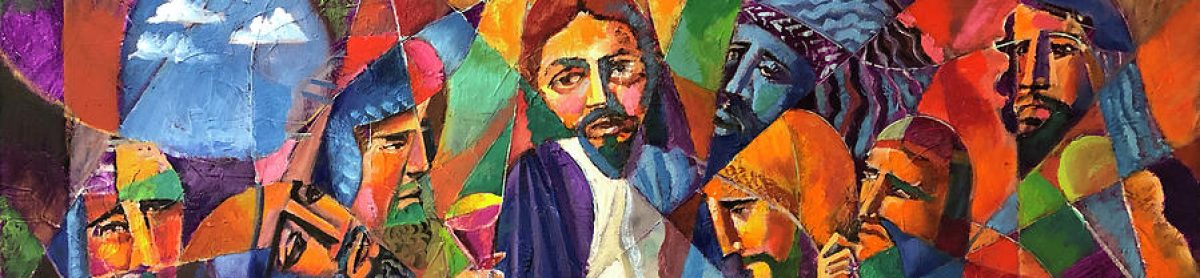
I need to briefly share what delusions are like. I’m going to flip the switch and flood the room with light, and watch the “critters” scuttle to find a hiding place.
I’m doing this to help heal myself, and for you to understand this awful state of mind.
First of all, let’s define things.
Delusion n.
A false belief held despite strong evidence against it; self-deception. Delusions are common in some forms of psychosis.
Delusion de·lu·sion n.
A false belief strongly held in spite of invalidating evidence, especially as a symptom of mental illness.
Typically, my delusions have a common core of pride or self-centered thinking. For instance, I have experienced all of these to a degree:
- A woman loves me and she is secretly trying to be with me. This is very flattering and egocentric. This one can really mess with your thought-life. (Ego.)
- I’m the center of the universe, people really do not exist, except when they come into my life or influence. [This one is a bit metaphysical.] See #7.
- I have special powers that ‘know” a person’s motives, plans and heart. I am hyper-discerning. The opposite can be true at times, where I become exposed to people, which necessitates me never leaving my room. I feel “naked” and of course, very uncomfortable.
- I get paranoid, thinking people are plotting with each other behind my back, working to destroy me. Chat rooms, and Facebook are focal points for me with this one, but not always. With this one I get really verbal, and I start zapping people. I guess because it’s the internet I can do this with impunity.
- Clocks are always at the top of the hour, like- 7:00 am. Or they are at the bottom of the hour, like 11:30 pm. I call this “chronosynchronism.” I believe this is evidence that my life is orchestrated, purposeful, and this is evidence I am very significant. This is my latest. And it really isn’t super disruptive.
- I can read secret messages in books meant for me. I also line up spaces in what I’m reading to form an unbroken line. I compulsively do this.
- The big one is this, I am in my form of “The Truman Show”. The universe is just a set and I am the only living thing out there. Everything is focused on me (of course).
- I hear voices sometimes, but mostly a radio or sometimes the “dot-dash-dot” of a telegraph. I think its trying to warn me in some code. It can be persistent. And it can be disruptive. Paranoid because my giftedness is the primary reason for the NSA to control me.
- My wife intends to poison me.
- Personal hygiene issues. Afraid of being murdered in the shower creates a super-phobia. I once went 6 weeks without showering. (I made my own eyes ‘water’, lol).
I guess all of these have one thing in common.
They are self-centered. They are unreasonable and illogical. They are compulsive. And yes, meds do work. And the above list? The delusions are only mild-to-moderate issues of delusional paranoia. There are so many Christians and non-Christians who have worse. I once met a man who seriously believed he was Jesus. (And no, I didn’t worship him).
As a believer working out his discipleship, I’ve discovered that humility and openness is always the way of keeping one tethered to reality. However, I have a fear that I will break loose and never come out again. I MUST live in “brokenness”. (So in a strange way, following Jesus Christ is easier.)
Also, I must be open to things that will invalidate my delusion. Even if I’m 99% convinced, that 1% will cause me to consider thinking through a scenario. Truth is your best friend when you are challenging a delusional paranoid. But it has to be gently applied. Life doesn’t have be lived this way. Also, delusions will often ‘morph’ and change and take on modified characteristics. This seems to be part of the mental illness, but can also indicate demonic oppression (or both even).
A psychiatrist should be informed in most cases. Very often meds will be necessary to get you through this time, but not always. But sometimes.
Praying for delusional behavior
People have prayed for me, more then I have prayed for myself. Your intercession bridges a gap over this illness. When you pray, you power up the energy cells and get instructions. It may mean wait, or proceed. Every person and situation is different.
“Do not believe that he who seeks to comfort you lives untroubled among the simple and quiet words that sometimes do you good. His life has much difficulty and remains far behind yours. Were it not otherwise he would never been able to find these words.”
Prayer is always the best approach.
So many delusions and so little time. They will vary from person-to-person. An active prayer may help, “Lord, may it be the real me who touches the real You.” Remember, Jesus stands at the right hand of his Father praying for you [which can’t be all bad].
Romans 8:34